Registration of clinical trials was first introduced as a way to combat publication bias and avoid the duplication of efforts in medical research. Since then, the registration of clinical trials has been deemed a requirement of publication by the International Committee of Journal Editors (ICJE) and various federal laws. However, the mere registration of a clinical trial does not guarantee its ultimate completion, nor publication.
In a new article published last month in PLoS Medicine, Speich and colleagues set out to better understand the prevalence and impact of non-registration, early trial discontinuation, and non-publication within the current landscape of medical research.
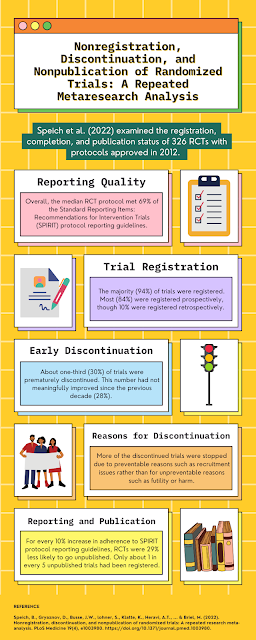
An update of previous findings published in 2014, the study examined 360 protocols for randomized controlled trials (RCTs) approved by Research Ethics Committees (RECs) based in Switzerland, the United Kingdom, Germany, and Canada. Of these, 326 were eligible for further analysis. The team collected data on whether the trials had been registered, whether sample sizes were planned and achieved, and whether study results were available or published. The team also assessed each of the RCTs for protocol reporting quality based on the Standard Protocol Items: Recommendations for Intervention Trials (SPIRIT) guidelines.
Overall, the included RCTs had a median planned sample size of 250 participants and met a median of 69% of SPIRIT guidelines. Just over half (55%) were sponsored by industry. The large majority (94%) were registered, though 10% were registered retrospectively. About half (53%) reported results in a registry, whereas most (79%) had published results in a peer-reviewed journal. However, adherence to reporting guidelines did not appear to the rate of trial discontinuation.
About one-third (30%) of RCTs had been prematurely discontinued, which indicated no change in this regard since the previous investigation of RCT protocols approved between 2000-2003 (28%). Most commonly, trials in the current investigation were discontinued due to preventable reasons such as poor recruitment (37%), organizational/strategic issues (6%), and limited resources (1%). A smaller proportion were discontinued due to preventable reasons such as futility (16%), harm (6%), benefit (3%), or external evidence (3%).
For every 10% increase in adherence to SPIRIT protocol reporting guidelines, RCTs were 29% less likely to go unpublished (OR: 0.71; 95% confidence interval: from 0.55 to 0.92), and only about 1 in every 5 unpublished trials had been registered.
The authors suggest that these findings implicate the need for investigators to report results of trials in registries as well as in peer-reviewed publications. Furthermore, future research may assess the utility of feasibility or pilot studies in reducing the rate of trial discontinuation due to recruitment issues. Journals can require trial registration as a requirement to publish.
Speich, B., Gryaznov, D., Busse, J.W., lohner, S., Klatte, K., Heravi, A.T., ... & Briel, M. (2022). Nonregistration, discontinuation, and nonpublication of randomized trials: A repeated research meta-analysis. PLoS Medicine 19(4), e1003980. https://doi.org/10.1371/journal.pmed.1003980. Manuscript available at the publisher's website here.