In the guideline development process, a panel should use a defined framework to consider multiple aspects of a clinical decision, including but not limited to the certainty of the underlying evidence, potential impact on resource use, or variability in the values and preferences of patients and other stakeholders. Such frameworks include the GRADE Evidence-to-Decision (EtD) format as well as others such as the "decision-making triangle" and Guidance for Priority-Setting in Health care (GPS Health).
To better understand the prevalence and use of these various frameworks within guidelines, Meneses-Echavez and colleagues systematically searched for guidelines and related guideline production manuals published between 2003 and May 2020. Items were screened and extracted by two independent authors, with a total of 68 full text documents included and analyzed.
Of these documents, most (93%) reported using a structured framework to assess the certainty of evidence, about half (53%) of which used GRADE or adapted systems based on GRADE (10%). Similarly, 88% of documents reported using a framework to rate the strength of recommendations, with about half (51%) using the GRADE approach. However, only about two-thirds (66%) of the included documents explicitly stated the process for formulating resulting recommendations.
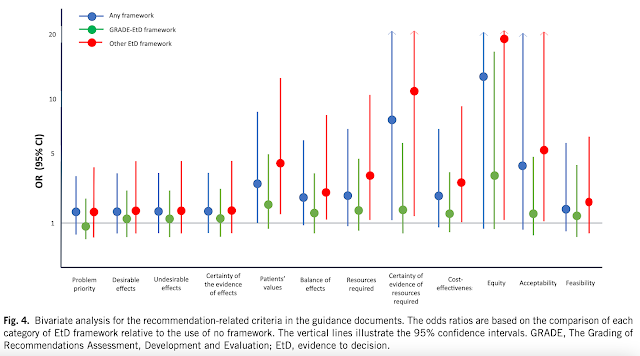
Finally, the GRADE framework was most commonly used for the evidence-to-decision, being cited in 42% of the included articles, with other reported frameworks including NICE (8%), SIGN (8%) and USPSTF (4%). Articles using the GRADE EtD framework reported considering more criteria than those using alternative approaches. The most commonly used criteria across documents included desirable effects (72%), undesirable effects (73%), and the certainty of evidence of effects (73%); the least commonly applied criteria were acceptability (28%), certainty of the evidence of required resources (25%), and equity (16%).
The use of any EtD framework was associated with a greater likelihood of incorporating perspectives (odds ratio: 2.8; from 0.6-13.8) and subgroup considerations (odds ratio:7.2; from 0.9-57.9), as was the use of GRADE compared to other EtDs (odds ratios: 1.4 and 8.4). These differences also affected whether justifications were reported for each judgment as well as the inclusion of notes to consider for the implementation of recommendations and for monitoring and evaluating recommendations.
The authors conclude that guidance documents stand to benefit from the more explicit reporting of how recommendations are formulated, from the initial grading of the certainty of underlying evidence to the consideration of how recommendations will affect various criteria such as resource use and equity. These changes, in the words of the authors, may "enhance transparency and credibility, enabling end users to determine how much confidence they can have in the recommendations; facilitate later adaptation to contexts other than the ones in which they were originally developed; and improve usability and communicability of the EtD frameworks."
Meneses-Echaves JF, Bidonde J, Yepes-Nuñez JJ, et al. (2022). Evidence to decision frameworks enabled structured and explicit development of healthcare recommendations. J Clin Epidemiol 150:51-62. Manuscript available at publisher's website here.